Everything you need to know about prostate cancer
Prostate Cancer > Diagnostic tools
Ancient diagnostic triad
For decades the diagnostic of prostate cancer has relied on a triad based on a clinical examination by digital rectal examination (DRE), a blood test with a prostatic specific antigen (PSA) and an imaging by transrectal ultrasound scan (TRUS).
• The digital rectal examination
Long before any other diagnostic test, the DRE has been the only way to detect prostate cancer. It allows to evaluate 33% of the prostate surface. The DRE is recommended by all the learned societies even if a meta-analysis on more the 8000 studies on the subject concluded that given the considerable lack of evidence supporting its efficacy it should not be recommended to perform routinely a DRE to screen for prostate cancer in the primary care (picture 16a) setting [8]. When a cancer is detected by DRE in 50% of the cases it has already move beyond the limit of the prostate. In oncology, the TNM (tumour – nodes – metastasis) classification is the core of the staging of any cancer. In prostate cancer the T is clinical and determined only by the DRE (table 1 and picture 16b).
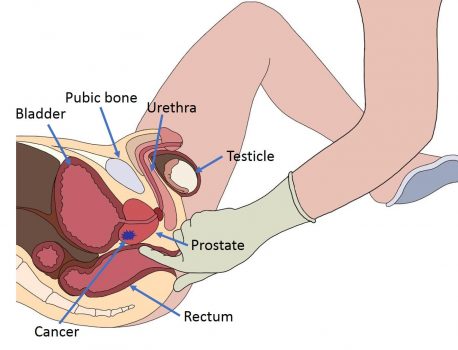
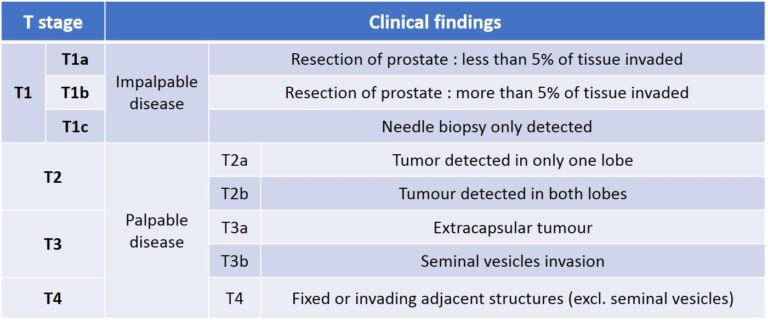
Table 1 : The tumour (T) parameter of the TNM classification of prostate cancer
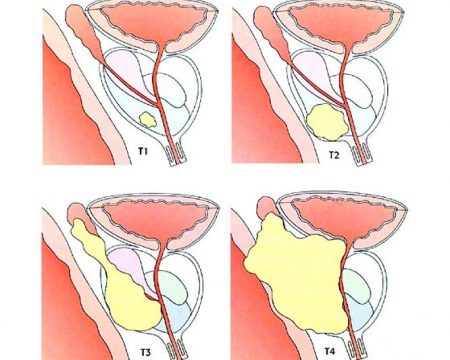
Picture 16 b : Presence of the tumour into the prostate according to the T stage
• PSA molecule
First characterised in the 70’s by Dr Richard Ablin for the purpose of rape conviction, the raise of PSA has been associated with prostate cancer in 1981 (picture 17). It is produced by the glandular cells either normal, hyperplastic or cancerous. Its concentration increases with age (table 2), presence of a benign prostatic enlargement, a cancer or an inflammation of the prostate called prostatitis from infectious origin or else. PSA is definitely not a tumour marker as every man with a prostate will have a certain concentration of PSA in his blood test. Even if the PSA has been criticized for its inaccuracy it is still necessary as a first step diagnosis (table 3).
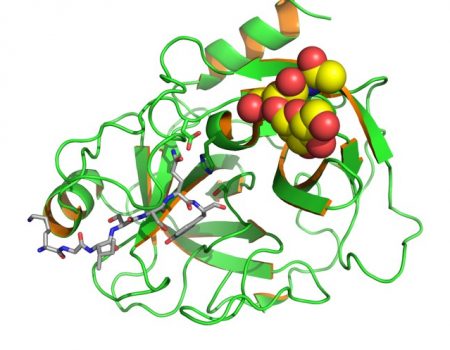
Picture 17 : 3D molecular structure of the Prostatic Specific Antigen (PSA)
Eventually there are many other derivatives to the PSA such as ProPSA, cPSA, BPSA, sPSA-N, Intact PSA, PSADT, PSAphi….
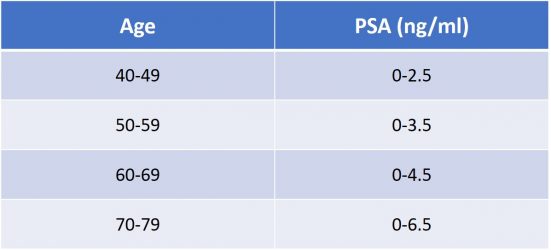
Table 2 : Acceptable range of PSA related to age
Many derivates of the PSA have been proposed :
-
PSA free/total
- Free form constitutes 5-40% of total PSA
- If the PSAF/T is below 0.1 there is an increased risk of PCa -
PSA velocity
– Represents the annual absolute increase in total PSA
– when PSA levels 4-10 ng/mL the acceptable increase is below 0.75 ng/ml/year -
PSA density
– The PSA density (PSAD) is the ratio PSA/prostate volume knowing that the production of PSA varies depending on type of prostatic tissue :
• normal prostate epithelium = 0.1 ng/mL • BPH = 0.3 ng/mL • PCa tissue = 3.5 ng/mL
– Therefore when the PSAD is above 0.15 the risk of prostate cancer is increased (figure 1)
– Conversely when the PSAD is below 0.1 the risk of prostate cancer is very low and it avoids to perform a new set of biopsies in 31% when the first set was already negative [9].
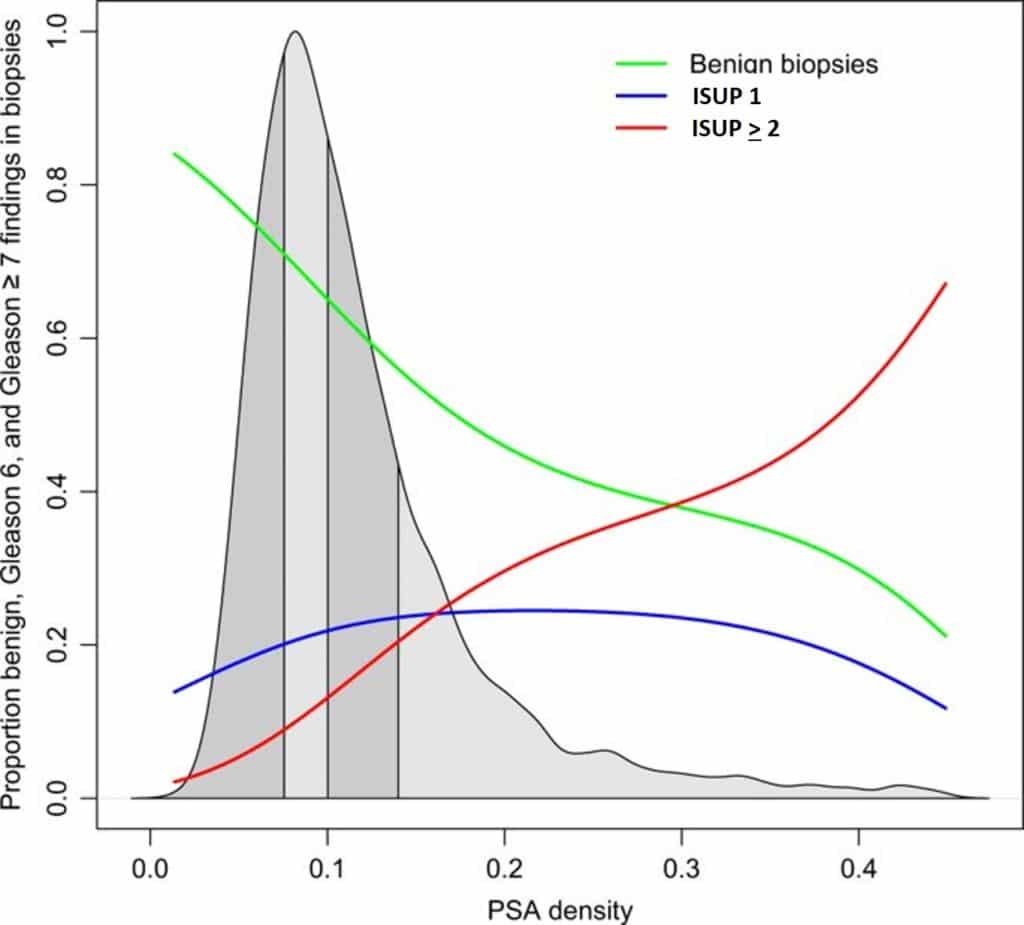
Figure 1 : Proportion of benign, ISUP 1 and ISUP > 2 related to PSAD
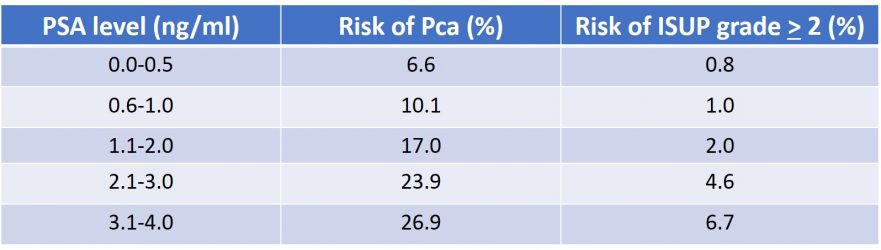
Table 3 : Probability of prostate cancer according to PSA blood test (source : EAU guidelines 2020)
• Transrectal ultrasound
The transrectal ultrasound scan (TRUS) has been described as early as 1968 by Watanabee et al. It is the best way to visualize the prostate by introducing the US probe into the rectum. The prostate being just in the front of the anterior rectal wall it gives a nice image of the prostate without any interference (picture 18). It has an interest to make the most accurate measurement of the prostatic volume however TRUS has no direct diagnostic relevance has the vast majority of prostate cancer are invisible on US scan. Meanwhile TRUS is still essential to perform the prostate biopsies and also for the planning of minimally invasive treatment such as focal therapy.
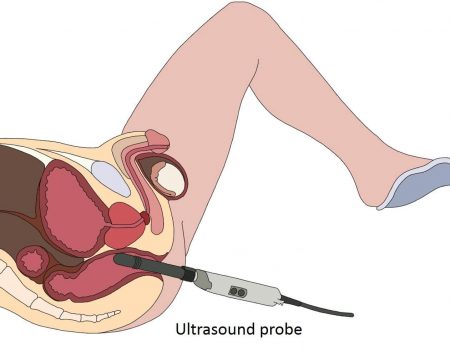
Picture 18 : Transrectal ultrasound (TRUS) with the immediate proximity of the prostate to the US probe (by B. Batard)
Multiparametric Magnetic Resonance Imaging (mpMRI)
The multiparametric Magnetic Resonance Imaging (mpMRI) is the diagnostic milestone of this 2 last decades in the expertise of prostate cancer. Nothing has changed the way of managing prostate cancer as much as mpMRI in the diagnostic as much as in the therapeutic field. Except for an obvious metastatic prostate cancer at its first presentation, no prostate cancer should be managed without a high-quality mpMRI.
Prostatic biopsies
The prostatic biopsies (PB) are the cornerstone of any prostate cancer treatment decision making. The technical improvement in the way of taking prostate biopsies has been revolutionized by the surge of mpMRI in the field. In the vast majority of the cases, the technology of fusion biopsy should not be anymore an option but an obligation as the accuracy brought by this new technology plunges prostate cancer management in the era of the 21th century.
With all these new knowledge and technologies now available no expert center would continue to diagnose and to treat prostate cancer as usual. The difference between a prostate cancer expert institution and a standard center does not rely anymore in the way you treat but rather how you diagnose patients. Indeed diagnostic accuracy has become the key element in every PCa management.


