Optional Treatments
Treatments > Prognosis and Follow-up
D’Amico classification
Adopted by major Urological associations such as the European Association of Urology (EAU) and the American Urological Association (AUA), since 20 years, the d’Amico classification is the main tool used to assess prognosis in prostate cancer [10]. The d’Amico classification is a simple useful tool which assess the 5-years recurrence rate after a local treatment. Others prostate cancer risk stratification systems such NCCN, NICE or ESMO are used. The d’Amico classification is based on 3 parameters : biological the PSA, pathological the ISUP score and clinical the tumour staging (T) of the TNM classification. Due to the shift of the previous Gleason score pathological classification to the ISUP score system and the importance of the percentage of positive biopsies in a set some modifications have been proposed mainly in the Intermediate Risk group (IR) to the d’Amico classification. Also in the Low Risk (LR) a subgroup so-called Very Low Risk has been identified on the base of <3 biopsy cores positive, ≤50% cancer in any core and PSA density <0.15 ng/mL/mL. In total instead of 3 initial risk groups an updated classification may include 3 groups of which the LR and the IR would be divided in 2 subgroups (table 19).
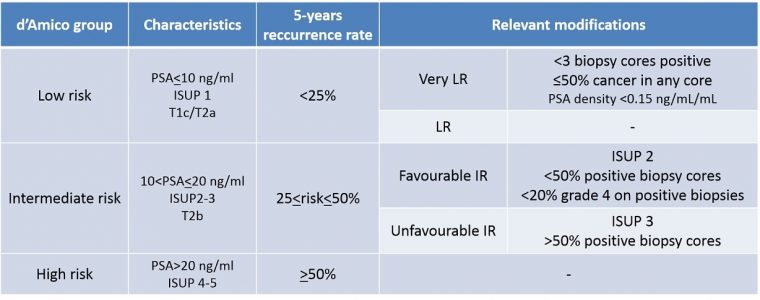
Table 19 : d’Amico classification updated
Follow-up
In Oncology, the follow-up is as important as any treatment strategy and in prostate cancer complete remission or full recovery is pronounced only after 10 years follow-up. Radiotherapists may differ from this definition and consider a 5-years period as sufficient. The classical prostate cancer follow-up depends on the therapeutic strategy. PSA blood test and digital rectal examination (DRE) are always part of the follow-up. Additionally when the prostate is still in place (radiotherapies, focal treatments or active surveillance) mpMRI and/or control biopsies may be part of the follow-up. In the vast majority of the cases recurrence is discovered by a steady increase of PSA so-called biochemical failure.
• Radical prostatectomy
When the prostate is removed mpMRI and control biopsies are not possible unless signs of local recurrence with an objective of salvage radiotherapy. Usually the follow-up sums up to a PSA blood test and a DRE every 3 months during 2 years then every 6 months during the 3 followings years then yearly until reaching 10 years follow-up. The tightened follow-up during the first 24 months is due to the high-risk during this particular period as 80% of all the recurrences in prostate cancer occur during this early post-treatment period. The PSA results should be and stay as low as possible around 0.01 ng/ml. When it reaches 0.2 ng/ml the recurrence is established (picture 82). Recurrences are exceptional after 10 years.
Most of recurrences are detected biologically by the PSA blood test. If the PSA increase rapidly soon (< 6 months) after the surgery usually the disease relapse is not local and the patient will need an exhaustive staging workup (chest-abdominal CT scan, bone scan and/or PET-scan) in order to show the extent of the disease when possible. If the PSA increases slowly after12-24 months most of the time it is a local recurrence and a salvage external beam radiation therapy (EBRT) strategy will rule out the cancer at the price of potential additional side effects. When a recurrence in IR and HR the combination surgery followed by EBRT works well.
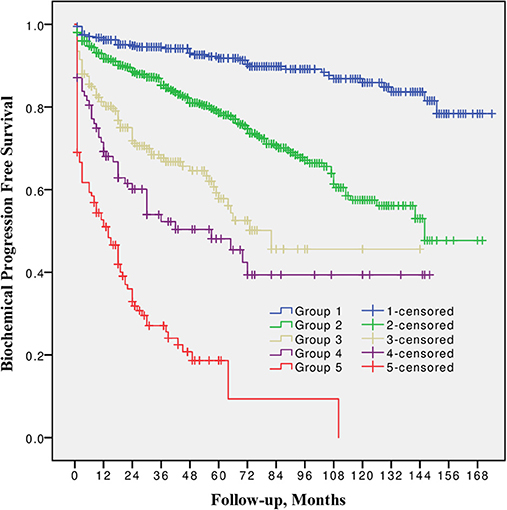
Picture 82 : Radical prostatectomy failure expressed by PSA reascencion (source : Milonas D. et al. Front. Oncol. 2019)
• Radiation therapies
As previously mentionned Radiotherapists rather consider the full recovery after a radiation therapy treatment at 5 years. Except salvage radiotherapy after radical prostatectomy, the difference between radiation therapies either external or brachytherapy or combined and radical prostatectomy is the conservation of the prostate in place. The follow-up may be altered in case of increased PSA with the realization of an mpMRI and control biopsies. However in most countries the usual follow-up is similar to the radical prostatectomy scheme. In case of brachytherapy when the procedure is performed by a combined Radiotherapist-Urologist team the follow-up is organized in rotation. The recurrence is established when the PSA value reached its lowest value after treatment so-called the nadir + 2 ng/ml [Phoenix definition] (picture 83).
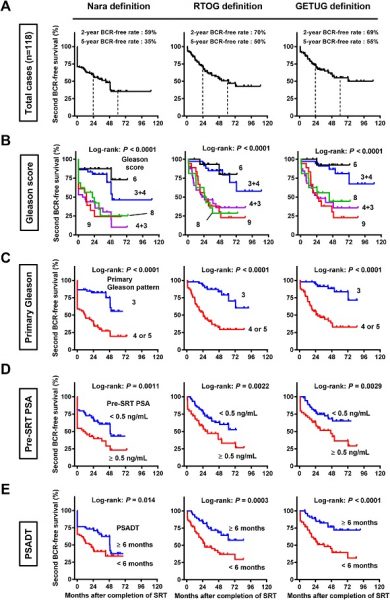
Picture 83 : Different failure definitions give different results (source : Miyake M. et al. Prostate International. 2019)
• Active surveillance
The follow-up is based on PSA blood test, DRE and biopsies. Even if mpMRI is a very accurate and an interesting tool for the time being it is not used routinely to assess a progression. Most of active protocol would recommend a PSA blood test and DRE every 3 months the 2 first years then every semester. Control biopsies are mandatory to check any pathological progression at 1 year and then every 3 years. The rythm of follow-up may change depending on the estimated risk of progression. A steady increase of PSA may trigger a radiological control by mpMRI before a new biopsy set in order to identify an eventual target (picture 50).
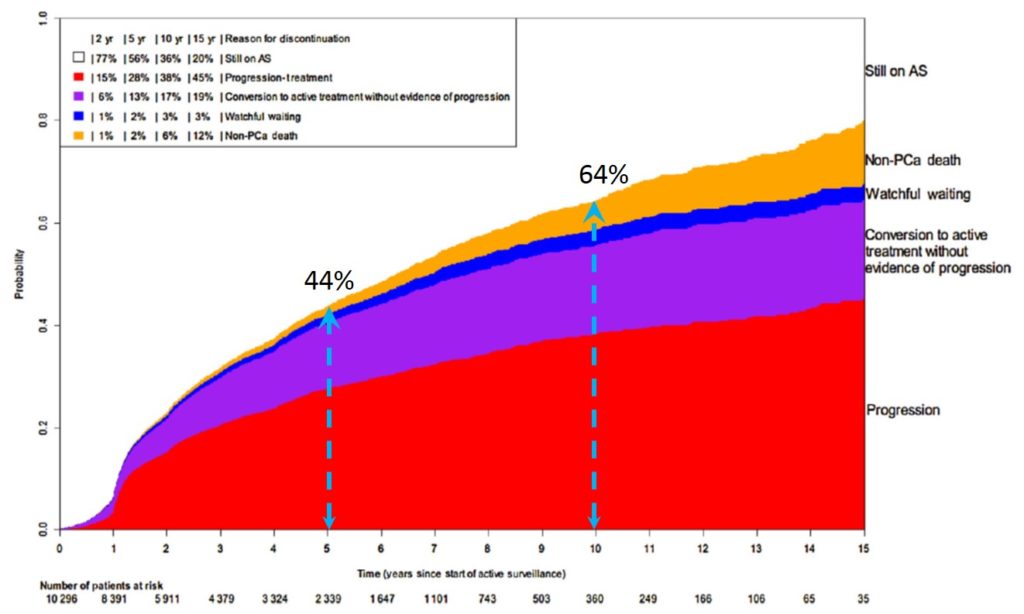
Picture 50 : Reasons and proportions of discontinuation of active surveillance (source : Movember GAP3 Consortium)
• Focal Therapy
As the most recent therapeutic strategy available in the prostate cancer field, the follow-up of focal therapies is based on Consensus groups constituted by the best expert in the field (picture 84). In Kyoto, in 2018, a Consensus group has proposed the most accomplished follow-up protocol based as follows : 1) PSA every 3 months for a year then every 6 months, 2) mpMRI at 6 and 18 months, 3) a combined biopsies set of randomised + targeted in the treated area at 6-12 months after the treatment [45]. Regarding the control biopsy after this first set the active surveillance protocol could be used as a model with new control biopsies every 3 years.

Picture 84 : Connecting experts knowledge to reach a consensus


