Everything you need to know about prostate cancer
Prostate Cancer > Diagnostic tools > Prostatic biopsies
The importance of the transrectal ultrasound scan
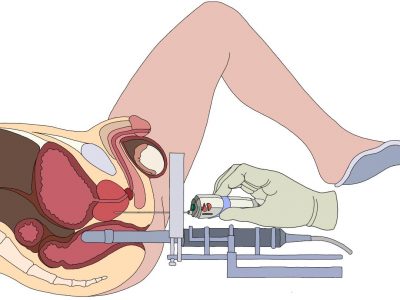
No diagnostic of prostate is confirmed without a pathological examination of prostate biopsies. Through the years the manner prostatic biopsies have been taken has dramatically changed with a huge impact on the diagnostic accuracy. Initially digitally-guided the surge of the transrectal ultrasound scan (TRUS) has represented the first revolution in the field (picture 24). From a situation where the whole procedure was performed in a blinded manner with the TRUS the prostate became visible. The 80’s were the beginning of the ultrasound-guided or TRUS-guided biopsies with the use of a transrectal probe. At the same time in the biological field the PSA test became available allowing an earlier diagnosis and changing irreversibly the management of prostate cancer.
Picture 24 : A first milestone in the prostate imaging approach (Liddell HT et al. J. Urol. 1986)
• Indication
Prostate biopsies are necessary in any man with a life expectancy of ten years or greater with an abnormal digital rectal examination (DRE) or an elevated PSA (usually above 4 ng/ml). In older men if the probability of an advanced or metastatic disease is high prostate biopsies may be needed before any palliative treatment.
• The technique
Except in very rare situations general anesthesia is not necessary and a local anesthesia is largely sufficient. They are different protocols for this procedure which takes place in the majority of the cases in an outpatient facility.
-
An enema to clean the rectum
Most of the time an enema is performed the day before or the same day by the patient to clean the rectum in order to improve the quality of the transrectal ultrasound images in an empty rectum and to reduce the concentration of bacteria and the risk of a prostate infection (acute prostatitis) when the biopsies are transrectal. Once the enema is introduced into the rectum the patient needs to wait 5 to 10 minutes before emptying his rectum (picture 25).
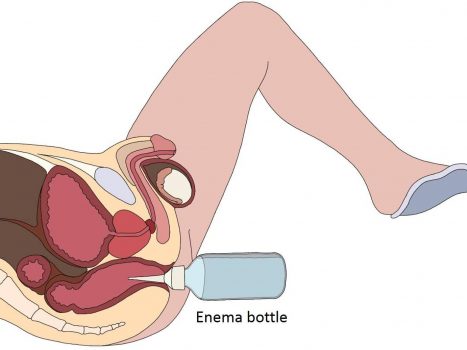
Picture 25 : Application of an enema few hours before the biospy procedure (by B. Batard)
-
Antibioprophylaxia
The antibioprophylaxia is a complicated word meaning that conversely to the antibiotherapy where the antibiotics are taken to fight an already active infection the antibiotics are used to avoid the surge of an infection. Indeed the introduction of a probe into the rectum and all the maneuvres around put the patient at a high risk of getting an acute prostatitis if the procedure is not covered by an antibiotic. Depending on the country, most of the time antibiotics from the quinolone or cephalosporine families are used (ofloxacine, ciprofloxacine, cefixime or else) (picture 26).

Picture 26 : Antibioprophylaxia to reduce the risk of acute prostatitis – To take orally 1-2 hours or intravenously just before the biopsy
-
Local anesthesia
TRUS prostate biopsies are an invasive examination. As such every discomfort caused by the procedure has to be reduced as much as possible. However the means used to reach that goal has to be proportional in terms of risks and medical expenses. For a first set of biopsies, except in very rare situations general anesthesia should never been proposed unless the patient insists not to have the biopsies performed under local anesthesia. The common rule is to use a local anesthetic (e.g. xylocaine) by transrectal injection (picture 27a) and/or intrarectal gel before starting to take the biopsies. With the surge of transperineal biopsies local anesthesia could also be performed through the perineum (picture 27b).
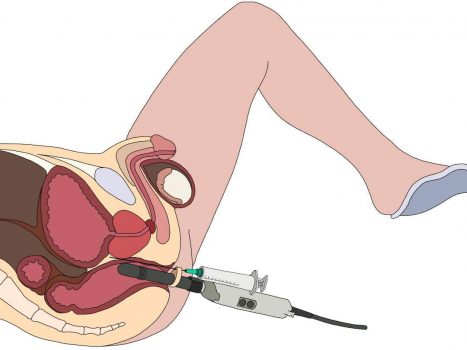
Picture 27a : Transrectal xylocaine injection (by B. Batard)
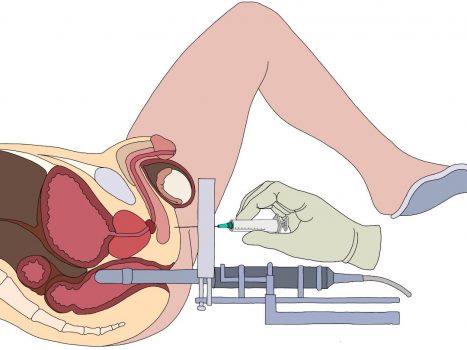
Picture 27b : Transperineal xylocaine injection (by B. Batard)
-
Examination position
Depending on your Urologists practice you may be laying on your back in a kind of “gynaecological” position so-called lithotomy position when men. Some Urologists would prefer the patient to lay on the side with bended knees (foetal position) (picture 28).

Picture 28 : Lateral decubitus position – only for transrectal biopsies
• Different sampling approach
Rapidly after starting to perform the biopsies by using the TRUS a standard mapping has been proposed on the base of six biopsies 3 in each lobe. After many studies have shown that this sampling was missing a certain proportion of cancer the so-called sextant biopsies scheme was proposed (pictures 29-30).
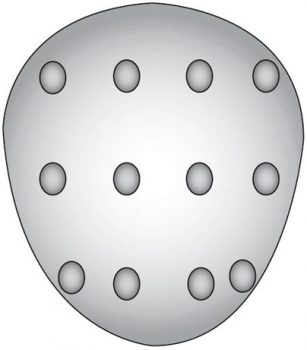
Picture 29 : 12 spots scheme applied without distinction amongst patients
-
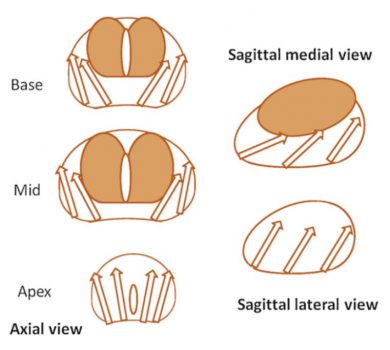
Standard or randomised biopsies
The sextant biopsies is the sampling of 6 core biopsies in each lobe with different schemes. It is called standard or randomised biopsies (SB or RB). For every patient the same scheme is applied without difference unless additional biopsies are performed on a palpable nodule. All the biopsies are performed on the faith of the TRUS which does not detect the cancerous lesion in the prostate. In a certain way SB/RB are performed blindly as the TRUS does not allow to detect the cancer lesions into the prostate. In the situation of the scenario proposed in the picture 31 even if the biopsies have been performed in the best state of art of standard biopsies and following accurately the recommended scheme the dangerous anterior lesion (in red in the left lobe) has been missed. Consecutively the patient will be falsely reassured by the negative results and the tumour will continue to progress. Here stands the revolution of the multiparametric MRI (mpMRI) and the following targeted biopsies. The cancer detection rate of SB/RB is around 20-30 %.
Picture 31 : 3D prostate with unreached anterior lesion (in brown)
-
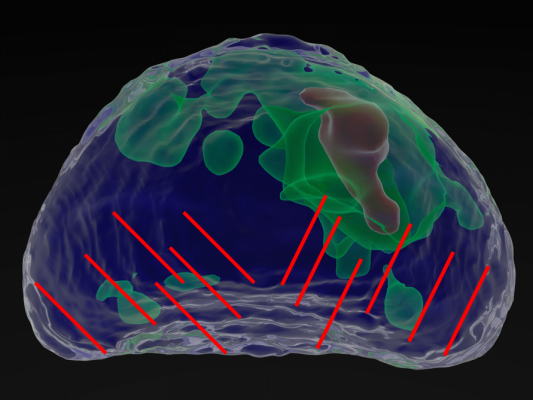
Targeted biopsies
The mpMRI is the milestone of this last 2 decades in the prostate cancer diagnostic expertise as it makes the invisible visible. This scientific breakthrough has changed the state of art of the management of prostate cancer. Where the clinic and the biology have failed the radiology is on the verge of overcoming the main pitfall of prostate cancer management : the overtreatment. By allowing a far more accurate and targeted sampling of the visible suspicious prostate lesions mpMRI has completely changed the level of accuracy of the reality of the disease into the prostate and therefore the way it should be treated. The better you know your enemy the more optimal option you choose to defeat the disease. For the time-being it is recommended by the learned societies to perform in addition to the targeted biopsies (usually 3 cores/lesion) an additional set of randomised biopsies. Indeed studies have shown that this combination of biopsies increases the detection rates by 5 to 7 % of significant cancers to reach up to 85-90 % in some expert centers.
-
TRUS Targeted Biopsies
As shown in the illustration (picture 32), with the help of software the lesion is localized into the prostate and then in realtime easily targeted with a biopsy gun (picture 33). The TRTB procedure is performed in the same conditions than SB however due to the high-resolution technology the time of the procedure is around 30 minutes.

Picture 32 : High resolution targeted biopsy procedure based on a MRI/US fusion system
-
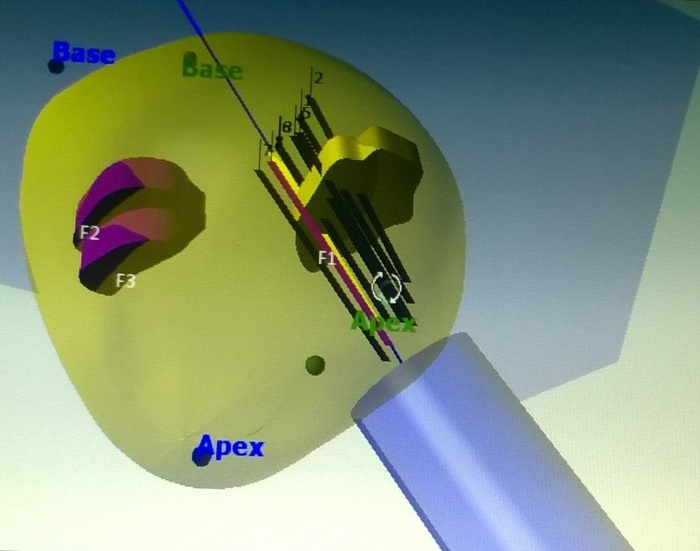
TransPerineal Targeted Biopsies
Transperineal targeted biopsies (TPTB) is the last medical innovation in the field. It relies on the same technology than the TRTB but with a different approach as the biopsies core are taken transperineally. TPTB need a different local anesthesia to avoid any pain during the procedure. The main interest of this approach is to reduce drastically the infectious risk. Indeed the needle of the biopsy gun will not anymore enter into the rectum with a huge amount of bacteria transported from the rectum to the prostate (picture 34). For this reason TPTB do not necessarily need antibioprophylaxia. When the mpMRI shows no prostatic lesion and the PSA continues to increase or the DRE is abnormal there is a possibility to perform transperineal biopsies using the Ginsburg protocol scheme in order to standardize in the best way the prostate sampling in these unusual situations (picture 35). Due to the elevated number of biopsy cores taken, for this last protocol more generally the procedure is performed under general anesthesia in an operating room.
Picture 34 : Sagittal view of transperineal targeted biopsies (by B. Batard)
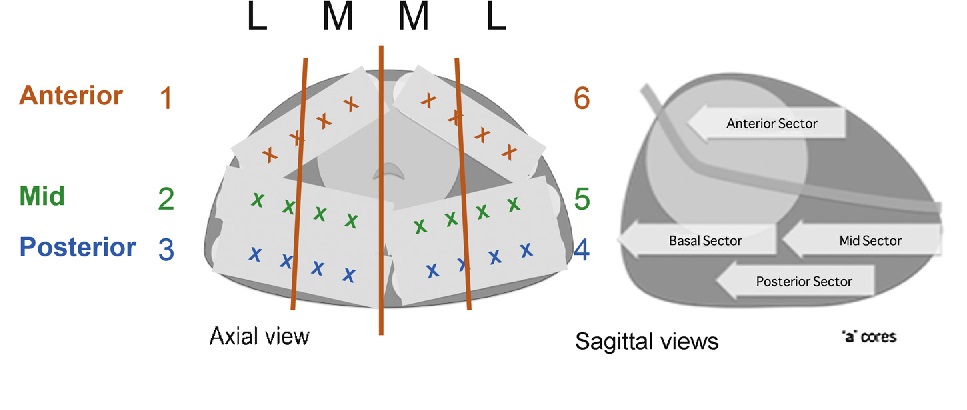
Picture 35 : Ginsburg protocol scheme (source : European Urology)


