Validated Treatments
Treatments > Validated Treatments > Surgery Radical Prostatectomy
Evolution of the technique
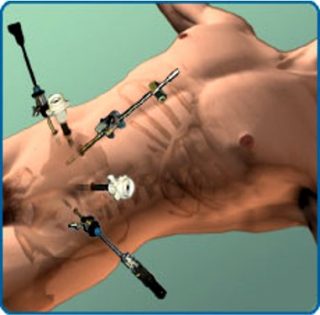
Radical prostatectomy has been around for more than 115 years. No treatment in the prostate cancer field has gathered some much experience. In April 1904 at the John Hopkins Hospital in Baltimore (USA) Dr H. Young and Dr. W.S. Halsted opened the way to the surgical radical treatment by removing entirely and for the first time a prostate by a perineal approach (picture 37). Nowadays very few centers are still performing perineal radical prostatectomies [PRP] (picture 38). At that time the mortality due to the radical prostatectomy culminated at 50%. In the 30’s after the surge of general anesthesia (GA) the abdominal surgery became possible with a retropubic approach still used today in some centers. For the next 50 years they were not particular surgical progress until Pr P. Walsh described a standardized technique with a nerve-sparing stage and a better bleeding control due to a more anatomical approach. The Walsh technique was the start of the golden age of radical prostatectomy which culminated at the end of the 20th century with the Barré-Chauveau technique, 2 French surgeons who used to perform the radical prostatectomy at 4 hands often in less than one hour (picture 39). At the same time a new approach was on its way with the surge of the laparoscopy in almost every field of the abdominal surgery (picture 40). Then again French surgeons confirm their expertise in the surgical prostate cancer field. Since 20 years and after a century of experience open radical prostatectomy (ORP) has been gradually superseded by the laparoscopic (LRP) with or without robot-assisted arms (RARP). It is important to underline that the removal of the prostate gland separates definitely the urinary and the male reproductive systems as the prostate is the junction between the urinary and genital tracts.
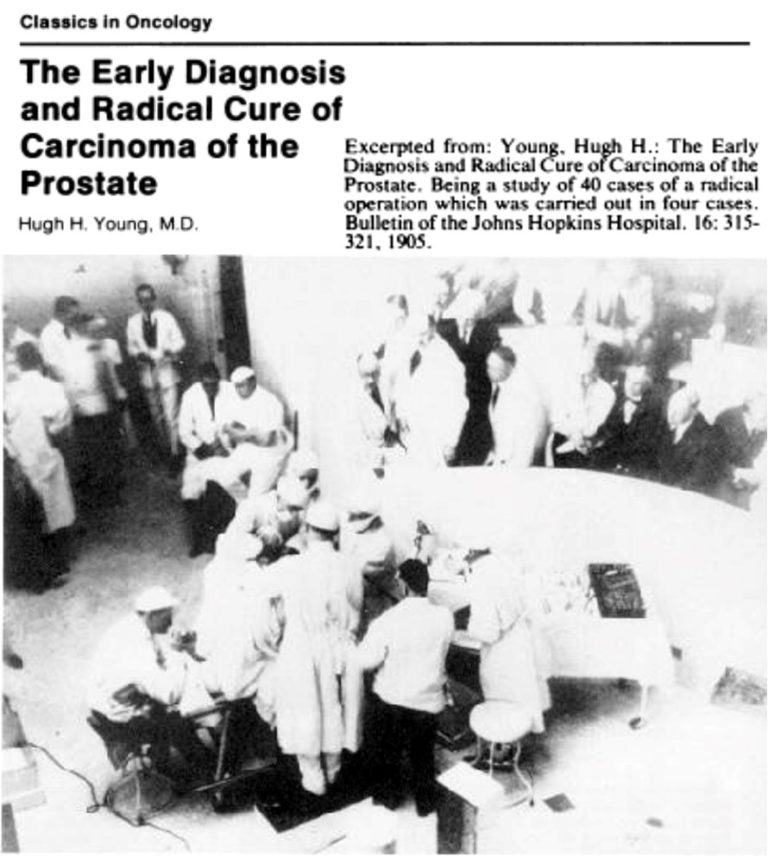
Picture 37 : The first radical prostatectomy at the John Hopkins Hospital (Baltimore, US) and the concomitant publication of the first serie of 4 cases
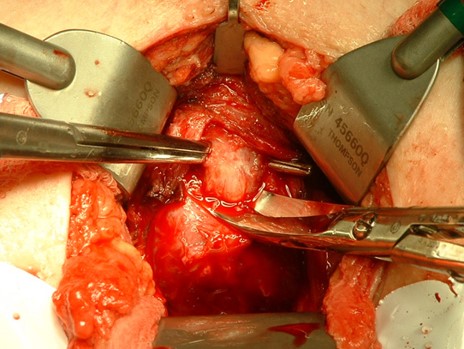
Picture 38 : Surgical site of a perineal radical prostatectomy
Surgical procedure
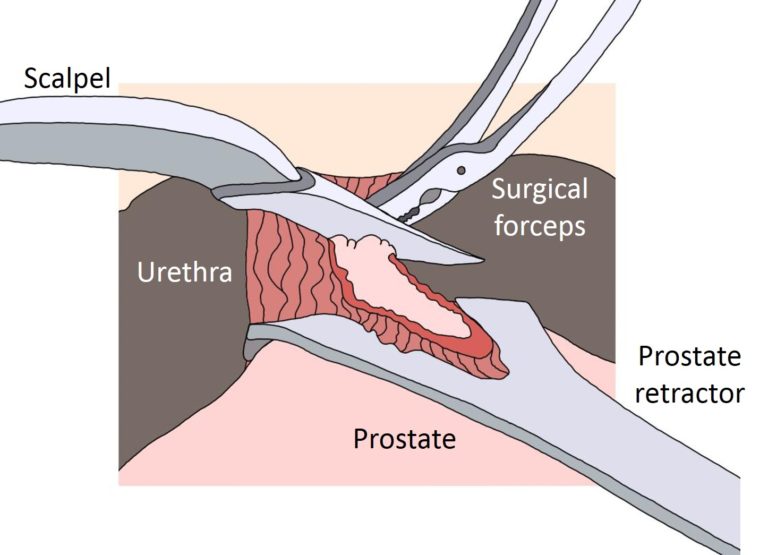
Radical prostatectomy whatever the approach open, laparoscopic or robot-assisted will always end with the complete removal of the prostate. As a matter of fact the surgery is rather the removal of the prostate and the adjacent seminal vesicles as a whole (picture 41). The main difficulty of this surgical procedure is due to its anatomical environment. In the front of the prostate the Santorini veinous plexus is at high risk of bleeding importantly. Below the prostate the narrow urinary sphincter can be easily harm by the surgery. Eventually the preservation of the invisible neurovascular bundles lying on each side of the prostate are more a bet than a mastered time of the surgical procedure. No technology will ever change the complex and intricated anatomy of the prostate and its closest surrounding structures (table 6). Particularly regarding the erection 25 % of men do not have simple neurovascular bundles but rather a wide neurovascular network lying on each lateral flank of the prostate which excludes any possible nerve-sparing approach. Before surgery the particular anatomy of the neurovascular bundles of a patient is not predictable.
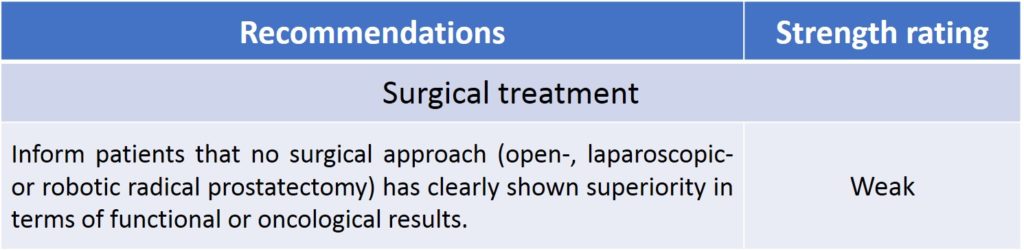
Table 6 : No difference in oncological or incontinence/erectile dysfunction results between open/laparoscopic/robotic approach (source : EAU guidelines 2020)
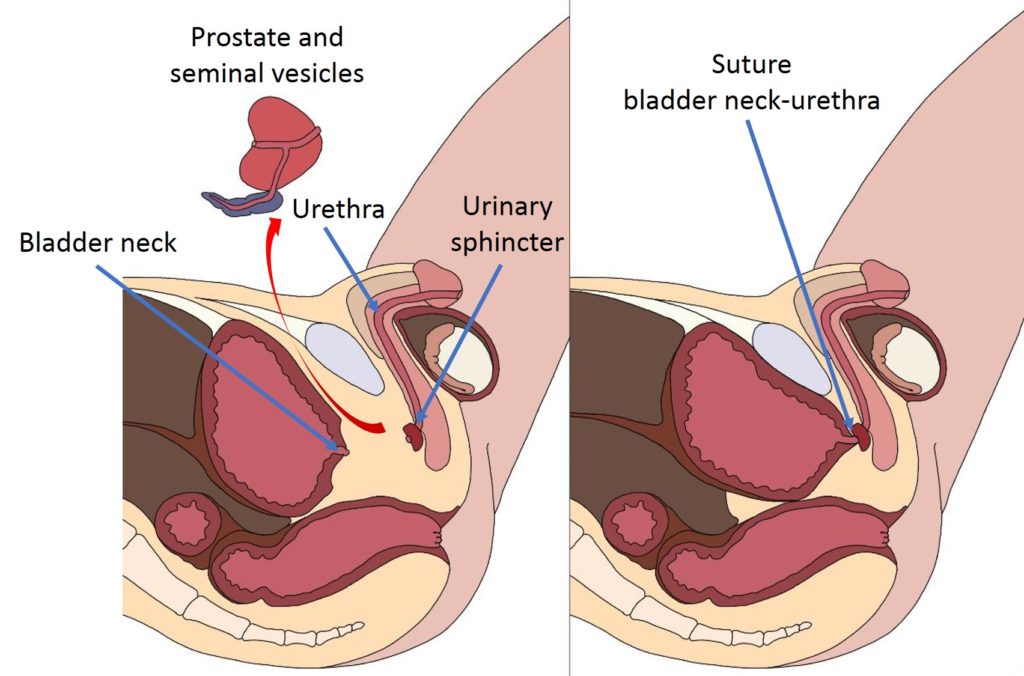
Picture 41 : Ablation of the prostate with immediate proximity of the urinary sphincter explaining the incontinence rate (by B. Batard)
Indications/Guidelines
Based on countless scientific studies, learned societies have regularly published guidelines to standardized in the best way the prostate cancer management. The most important urological associations such the European Association of Urology (EAU), the American Urological Association (AUA), the Chinese Urological Association (CUA) or the Confederacion Americana de Urologia (CAU) in Latin America vastly agreed on the indication of radical prostatectomy. Except in the Low Risk prostate cancer where overtreatment is still hitting hard, it is generally accepted that in every localized prostate cancer and in some locally advanced stage radical prostatectomy is a validated treatment when not the gold standard (table 7). However the striking reality is that for decades radical prostatectomy has been performed without any scientific evidence of its efficacy against the increased mortality due to prostate cancer. Even worst all the important studies regarding the impact of radical treatments on the overall survival [OS] (death form any cause) or cancer specific survival [CSS] (death from prostate cancer) have shown no impact of radical prostatectomy compared to a simple surveillance (table 8). However beyond the very important criteria of quantity of life the same studies have shown at midterm a real potential of progression of the disease with the onset of metastasis when no physical treatment was applied and a clear impact on the quality of life associated to radical treatments.
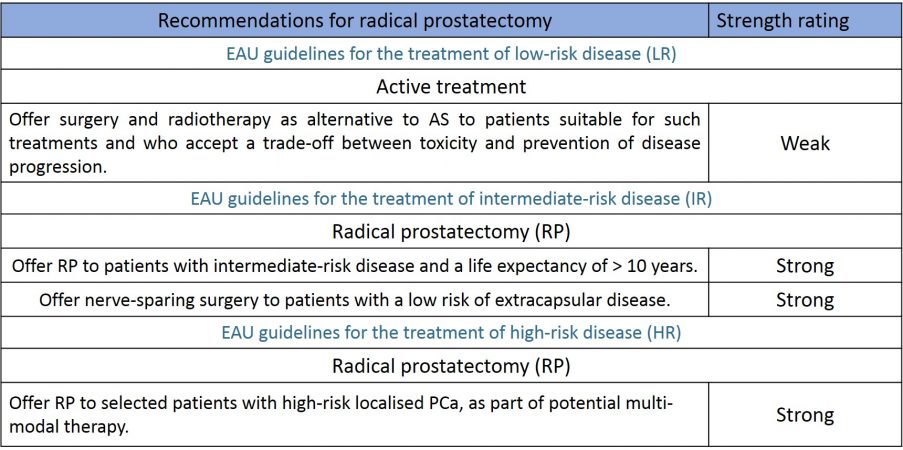
Table 7 : Recommendations of the EAU regarding the indication of radical prostatectomy in the different risk groups (source : EAU guidelines 2020)
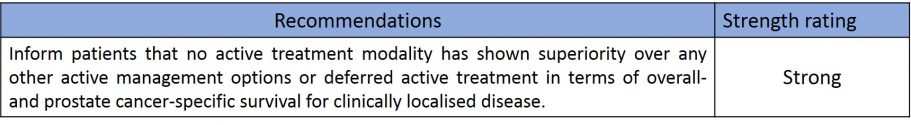
Table 8 : Strong scientific evidence of the absence of efficacy of radical treatments compared to simple surveillance on mortality (source : EAU guidelines 2020)
Results
After decades of practice radical prostatectomy in expert centers has reached a level of excellence. The aim of the surgery is to remove completely the cancer and to avoid as much as possible the principal side-effects which are incontinence and erectile dysfunction. By means of the most reliable studies in the field and with a long follow-up the efficacy of radical prostatectomy to avoid death due to prostate cancer is available (Table 9). Regarding the side-effects the ProtecT study has shown roughly around 20 % incontinence and 80 % erectile dysfunction (video 4).
Video 4 : Undeniable scientific evidence
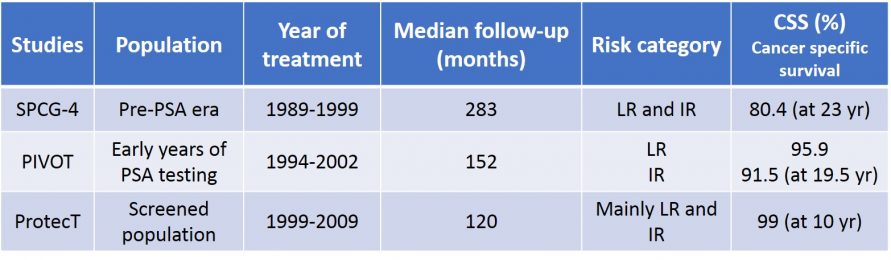
Table 9: Mortality rate after radical prostatectomy in the 3 most reliable studies in the field (source : EAU guidelines 2020)
Radical prostatectomy and Evidence Based Medecine
Three scientific studies (SPCG-4, PIVOT an ProtecT) of the highest level so-called randomised clinical trial (RCT) have compared on a long period of time (between 10 and more than 25 years) radical prostatectomy or radiotherapy with a surveillance protocol (active monitoring). For patients above 65 years, the results have been the same for the 3 RCTs showing no difference on the main criteria of overall survival (OS) (see videos-PPTs linked to each studies). Furthermore for the 2 more recent studies (PIVOT and Protect) performed during the PSA-era there were no advantage in OS or Cancer Specific Survival (CSS) to surgery or radiotherapy over active monitoring whatever the age of the patient [11-13]. Also noteworthy, the patient’s profile of the SPCG-4 study is not anymore valid compared to the present standard of care and in particular a PSA value up to 50 ng/ml. Selected on more up-to-date criteria SPCG-4 would probably show similar results compare to PIVOT and ProtecT studies.
The populations of this studies were mainly low-risk and intermediate-risk prostate cancer except for the ProtecT study with a component of high-risk prostate cancer patients. Noteworthy the same studies have shown at mid-term a real risk of progression toward a metastatic disease as high as twice when no physical treatment has been delivered.


